Last Updated on 08/02/2026 by Admin
Comprehensive Insights into Causes of Sudden Hearing Loss
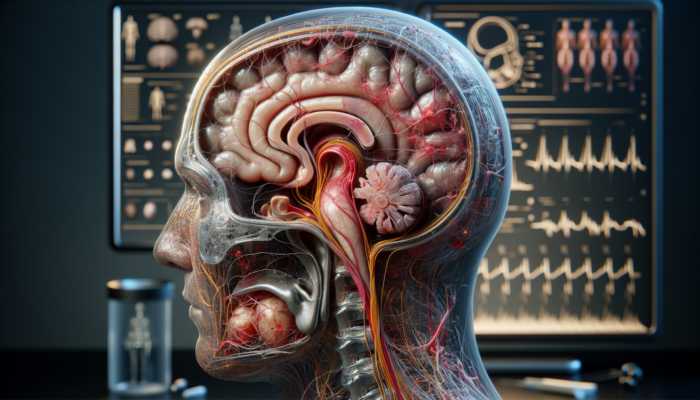
What Key Factors Lead to Inner Ear Complications?
Sudden hearing loss often stems from a variety of complications within the inner ear. Factors such as viral infections and blockages can severely impact auditory nerves, resulting in rapid onset of symptoms. For example, research indicates that many cases of sudden hearing loss are linked to viral infections, where patients report abrupt changes in their hearing within days of contracting a virus. This highlights the critical importance of seeking timely medical intervention to address these issues.
The effects of these factors are significant, as the inner ear is essential for processing sound. When it is disrupted by inflammation or physical blockage, auditory signals fail to properly reach the brain, leading to immediate hearing challenges. Conditions such as labyrinthitis and vestibular neuritis can cause acute hearing loss, underscoring the necessity for awareness regarding potential inner ear disorders.
What Common Everyday Triggers Cause Hearing Loss?
Day-to-day activities expose individuals to numerous triggers that can precipitate sudden hearing loss. Chronic exposure to loud noises, whether from concerts, industrial machinery, or personal audio devices, can damage delicate hair cells within the cochlea, resulting in an immediate reduction in hearing ability. Additionally, physical trauma, such as a head injury, can disrupt normal ear function, leading to swift hearing impairments.
Understanding these triggers enables individuals to adopt preventive measures. For instance, attending concerts or loud events without adequate ear protection can significantly increase the risk of irreversible hearing loss. Recognizing these hazards and the potential for early intervention is essential for ensuring auditory health and mitigating further complications.
How Do Environmental and Lifestyle Choices Affect Hearing Health?
Various environmental and lifestyle choices can influence the risk of sudden hearing loss by placing stress on the auditory system. Factors such as pollutants, excessive noise, and poor dietary habits are significant contributors to the overall risk profile for hearing issues. Being conscious of these factors is crucial for effective prevention and proactive management of auditory health.
- Exposure to noise pollution
- Smoking and tobacco use
- Chronic stress levels
- Poor nutrition and diet
- Exposure to harmful chemicals
- High alcohol consumption
- Lack of regular health check-ups
- Obesity and sedentary lifestyle
These lifestyle choices and environmental exposures can heighten risks, emphasizing the importance of an integrated approach to maintaining auditory health. By adopting healthier habits and minimizing exposure to harmful elements, individuals can significantly reduce their risk of experiencing sudden hearing loss.
How Does Sudden Hearing Loss Develop?
What Is the Impact of Vascular Issues on Hearing Loss?
Vascular issues, particularly disruptions in blood flow, play a pivotal role in the development of sudden hearing loss. When the inner ear is deprived of oxygen-rich blood, this can lead to rapid sensory damage. This phenomenon is often observed in patients with vascular disorders or those experiencing sudden fluctuations in blood pressure.
Seeking immediate medical attention is crucial, as prompt intervention can help prevent irreversible damage. Symptoms such as sudden deafness or persistent ringing in the ears (tinnitus) may indicate the urgent need for a comprehensive evaluation. Treatments often focus on addressing the underlying vascular concerns to restore adequate blood flow, highlighting the vital connection between cardiovascular health and auditory function.
What Symptoms Are Associated with Autoimmune Responses?
Autoimmune conditions can also lead to sudden hearing loss by causing inflammation that abruptly affects auditory structures. Symptoms often linked to autoimmune responses include tinnitus, vertigo, and a sudden drop in hearing ability. The body’s immune system can mistakenly target the inner ear, resulting in rapid changes to auditory health.
Understanding this connection is critical for individuals with existing autoimmune disorders or those experiencing symptoms that may indicate hearing issues. Early diagnosis and appropriate management are vital. Treatments may include anti-inflammatory medications and immunotherapy aimed at reducing inflammation, thereby aiding in the preservation of hearing abilities.
What Patterns Exist in the Onset and Progression of Hearing Loss?
Sudden hearing loss typically manifests unexpectedly, with symptoms escalating rapidly due to underlying physiological changes. Many patients describe a swift decline in their hearing abilities, often accompanied by other auditory disturbances. This unpredictable onset emphasizes the necessity of immediate evaluation by healthcare professionals.
As symptoms progress, seeking prompt medical intervention can be transformative. Evaluation methods may include audiometric testing and imaging studies to uncover the root causes of hearing loss. Recognizing the patterns in onset and progression empowers healthcare providers to implement timely and targeted treatment strategies, ultimately improving patient outcomes.
What Infectious Agents Are Linked to Hearing Loss?
Infectious agents, both viral and bacterial, can contribute to sudden hearing loss by causing inflammation in the inner ear or damaging the auditory nerve. Conditions such as otitis media and viral infections like mumps and measles can lead to rapid auditory changes that often require immediate antiviral or antibiotic treatment. The urgency lies in mitigating potential permanent effects and restoring hearing function.
Timely diagnosis is essential when infectious causes are suspected. Treatment options may include medications to combat the infection along with supportive therapies to manage symptoms effectively. Understanding these infectious pathways is critical for ensuring effective intervention and recovery from sudden hearing loss.
Expert Insights into the Causes of Sudden Hearing Loss
What Do Experts Say About Autoimmune Factors in Hearing Loss?
Experts in the field assert that autoimmune responses significantly contribute to sudden hearing loss through various inflammatory processes. This insight stresses the importance of managing underlying autoimmune conditions effectively. Clinical guidelines recommend regular monitoring of inflammation levels and adapting treatment strategies to address these challenges appropriately.
Actionable steps for individuals experiencing autoimmune issues may include dietary changes aimed at reducing inflammation, following prescribed treatment plans diligently, and closely monitoring auditory health. Establishing a comprehensive management plan is essential for minimizing the risks associated with sudden hearing loss.
How Are Neurological Connections Explained in Hearing Loss?
Neurological factors, such as nerve damage, are frequently highlighted by specialists as potential causes of sudden hearing loss. Understanding the relationship between the nervous system and auditory function can clarify how hearing capabilities may be compromised. Common diagnostic tools recommended by experts include audiograms, CT scans, and MRI imaging to assess structural integrity.
- Audiometric testing to evaluate hearing thresholds
- Imaging studies to analyze structural anomalies
- Electrophysiological tests to assess nerve function
- Blood tests to identify underlying conditions
These diagnostic tools are crucial for providing a deeper understanding of the neurological connections involved in hearing loss and paving the way for targeted interventions that address specific underlying issues.
What Are Trusted Methods for Evaluating Hearing Loss?
Thorough assessments recommended by medical experts are essential for accurately identifying the causes of sudden hearing loss. These evaluation methods uncover underlying issues that may contribute to auditory dysfunction. A comprehensive approach incorporates detailed patient history, physical examinations, and targeted diagnostic testing.
Expert analysis shows that pinpointing the root cause facilitates targeted treatments, leading to better outcomes for patients. Understanding the variety of evaluation techniques empowers individuals to seek appropriate care, ensuring timely interventions that can effectively preserve hearing function.
How Do Viral Infections Contribute to Hearing Loss?
Experts recognize viral infections, such as those caused by herpes or influenza, as significant contributors to sudden hearing loss. These infections can damage inner ear structures and disrupt normal auditory processing. Consequently, antiviral therapies are often recommended as part of the treatment plan for individuals experiencing hearing loss linked to viral etiologies.
Moreover, preventive vaccines can play a crucial role in reducing the incidence of viral infections known to adversely affect auditory health. Educating individuals about the importance of vaccination and early intervention can dramatically enhance hearing outcomes and overall well-being.
What Role Do Genetic and Environmental Factors Play?
Specialists analyze the interplay between genetic predispositions and environmental factors in exacerbating sudden hearing loss. Genetic research has revealed specific gene mutations that may increase susceptibility to auditory dysfunction. Therefore, genetic counseling can offer significant benefits for patients with a family history of hearing loss.
Additionally, implementing strategies to reduce environmental exposure, such as minimizing noise pollution and avoiding harmful chemicals, can greatly mitigate risks. Adopting a proactive approach empowers individuals to take control of their hearing health, effectively lowering the likelihood of sudden hearing loss.
Research-Based Insights into Causes of Sudden Hearing Loss
What Are the Key Mechanisms Behind Ear Damage?
Research has identified mechanisms such as pressure changes that can lead to sudden hearing loss by directly impacting the cochlea. For example, studies demonstrate that individuals who experience abrupt altitude changes may suffer auditory disturbances due to fluctuating pressure levels, which can result in sensory loss.
Real-world examples underscore the importance of understanding these mechanisms. By recognizing how pressure dynamics affect the inner ear, individuals can take preventive measures when engaging in activities such as flying or scuba diving, thereby safeguarding their hearing health.
How Do Underlying Health Issues Contribute to Hearing Loss?
Underlying health conditions can exacerbate sudden hearing loss due to the interconnected nature of bodily systems. Research findings indicate correlations between conditions like diabetes, hypertension, and auditory dysfunction, reinforcing the need for a holistic approach to overall healthcare.
Individuals with chronic health issues should remain vigilant about monitoring their auditory health, as these conditions can significantly impact hearing capabilities. Understanding this relationship can lead to better management strategies that address both hearing health and overall well-being.
What Preventive Insights Have Studies Revealed?
Studies highlight various strategies to mitigate the causes of sudden hearing loss through lifestyle modifications. Experts emphasize implementing evidence-based approaches such as practicing noise reduction, engaging in regular auditory check-ups, and maintaining a balanced diet rich in essential nutrients for ear health.
By adopting these preventive insights, individuals can significantly lower their risk of sudden hearing loss and foster long-term auditory health. Education and awareness about these strategies are vital for promoting proactive measures in hearing conservation.
What Is the Role of Genetics in Sudden Hearing Loss?
Genetic research emphasizes the importance of hereditary factors in sudden hearing loss, with specific gene mutations implicated in maintaining cochlear health. Individuals with a family history of hearing loss may be at a heightened risk, underscoring the need for genetic counseling and vigilance regarding potential risks.
Studies provide valuable insights into familial risks and emerging genetic therapies, offering hope for improved management and prevention strategies. Understanding the genetic landscape of hearing health empowers individuals to seek appropriate interventions and enhance their auditory well-being.
What Emerging Therapies Are Being Developed for Hearing Loss?
Advancements in medical research have led to promising new therapies for sudden hearing loss, including targeted medications and regenerative techniques. Evidence from clinical trials demonstrates the effectiveness of these therapies in restoring hearing, emphasizing the significance of timely intervention based on accurate cause identification.
As research continues to evolve, embracing these emerging therapies may open new avenues for effectively managing and potentially reversing sudden hearing loss, highlighting the importance of ongoing advancements in auditory health.
What Are the Key Triggers for Sudden Hearing Loss?
How Do Harmful Elements Trigger Hearing Loss?
Triggers such as chemical irritants and loud noises can lead to sudden hearing loss by damaging sensitive ear structures. Recognizing these harmful elements is essential for adopting protective measures early on. Examples of detrimental exposures include industrial chemicals, loud machinery, and certain medications.
Individuals working in high-risk environments must prioritize hearing protection to minimize exposure. By becoming aware of these triggers, one can take proactive steps to safeguard their auditory health, ensuring long-term well-being and preventing sudden hearing loss.
What Preventive Measures Can Be Taken to Mitigate Risks?
Implementing effective preventive measures, such as routine check-ups, can help counteract the triggers associated with sudden hearing loss. Engaging in regular auditory assessments allows individuals to monitor their hearing health and identify potential issues early. Practical steps, such as using earplugs in loud settings and avoiding prolonged exposure to harmful noise, can significantly reduce risks.
Creating awareness about these preventive strategies empowers individuals to take charge of their auditory health proactively. By integrating these measures into their daily routines, individuals can work towards preserving their hearing function and enhancing their overall quality of life.
What Is the Long-Term Impact of These Triggers?
Ongoing effects from various triggers may lead to permanent hearing loss if not addressed promptly, underscoring the importance of proactive measures against sudden hearing loss. Individuals exposed to loud noise over extended periods without sufficient protection are particularly at risk for irreversible damage.
Focusing on adaptive strategies, such as engaging in quieter hobbies or employing soundproofing measures, can help mitigate the long-term impacts of these triggers. Prioritizing auditory health is essential for maintaining sound hearing and preventing further deterioration over time.
How to Prevent and Manage Sudden Hearing Loss
What Strategies Facilitate Early Detection of Hearing Issues?
Early detection of hearing problems involves being alert to warning signs such as muffled sounds or difficulties in understanding speech. Recognizing these signs enables individuals to seek timely medical intervention, which can significantly halt the progression of sudden hearing loss.
Regular auditory assessments should be included in routine health check-ups, especially for individuals at greater risk. By remaining vigilant about changes in hearing ability, one can effectively preserve their hearing function and address potential issues before they escalate.
What Adaptive Techniques Aid in Recovery from Hearing Loss?
Adaptive techniques, such as sound therapy, play a vital role in managing sudden hearing loss by retraining the brain to process auditory information more effectively. These approaches focus on rehabilitation and can greatly enhance daily life and auditory capabilities.
Incorporating sound therapy into recovery plans can promote neural plasticity, allowing individuals to adapt to changes in their hearing. Engaging in consistent therapeutic practices fosters resilience in auditory health, empowering those affected to navigate their auditory challenges more effectively.
What Ongoing Maintenance Approaches Should Be Followed?
Ongoing maintenance approaches encompass regular health monitoring to address potential causes of hearing loss. Consistent check-ups with audiologists can ensure sustained hearing health through proactive measures, such as adjusting hearing aids or exploring new treatment options as they become available.
By prioritizing ongoing maintenance, individuals can manage their auditory health more effectively. This proactive approach not only preserves hearing function but also enhances overall quality of life, highlighting the significance of continuous engagement with healthcare professionals.
What Pharmacological Treatments Are Available for Hearing Loss?
Pharmacological treatments for sudden hearing loss often involve the administration of steroids and other medications aimed at reducing inflammation in the inner ear. When administered promptly, these interventions can help preserve or restore hearing function, minimizing potential complications.
Regular medical supervision is vital to monitor the effectiveness of these treatments and address any side effects. By adhering to prescribed regimens and maintaining open communication with healthcare providers, individuals can significantly enhance their chances of a successful recovery from sudden hearing loss.
What Lifestyle and Environmental Changes Can Help Protect Hearing Health?
Making lifestyle changes, such as avoiding exposure to loud noises and maintaining a balanced diet rich in antioxidants, can play a crucial role in preventing sudden hearing loss. Environmental modifications, such as employing ear protection in noisy settings, support long-term auditory health and reduce associated risks.
Additionally, incorporating stress management techniques into daily routines can further alleviate potential risk factors for hearing loss. By taking an integrated approach to lifestyle and environmental factors, individuals can foster better auditory health and promote resilience against sudden hearing loss.
Frequently Asked Questions About Sudden Hearing Loss
What is sudden hearing loss?
Sudden hearing loss refers to an unexpected and rapid decrease in hearing ability, often occurring within a span of days or even hours. It can be partial or complete and may affect one or both ears, necessitating immediate medical evaluation.
What causes sudden hearing loss?
Common causes of sudden hearing loss include viral infections, physical trauma, autoimmune disorders, vascular issues, and exposure to loud noises. Identifying the underlying cause is essential for effective treatment.
How can I prevent sudden hearing loss?
Preventing sudden hearing loss involves avoiding exposure to loud noises, maintaining a healthy lifestyle, managing stress, and regularly checking your hearing health with professionals.
Is sudden hearing loss reversible?
In some instances, sudden hearing loss can be reversible, particularly if treated promptly. However, the extent of recovery often depends on the underlying cause and the timeliness of medical intervention.
What are the symptoms of sudden hearing loss?
Symptoms can include a rapid decrease in hearing ability, muffled sounds, ringing in the ears (tinnitus), and sometimes vertigo. These symptoms may vary in intensity and duration.
When should I see a doctor for sudden hearing loss?
You should seek medical attention immediately if you experience sudden hearing loss. Timely medical evaluation is crucial for identifying the cause and initiating appropriate treatment.
Are there any risk factors for sudden hearing loss?
Risk factors include age, exposure to loud noises, certain medical conditions (such as diabetes), and a family history of hearing loss. Recognizing these factors can help mitigate risks effectively.
What treatments are available for sudden hearing loss?
Available treatments may include medications like corticosteroids to reduce inflammation, sound therapy, hearing aids, and in some cases, surgery. The treatment plan will depend on the underlying cause determined by a healthcare professional.
How can lifestyle changes impact hearing health?
Adopting healthier lifestyle choices, including a balanced diet, regular exercise, and stress management, can significantly enhance overall auditory health and decrease the risk of sudden hearing loss.
Can sudden hearing loss occur in both ears?
Yes, while sudden hearing loss often affects one ear, it can also occur in both ears simultaneously. If bilateral sudden hearing loss occurs, it is crucial to seek immediate medical attention for proper evaluation and treatment.
Join the conversation on X!
The post Causes of Sudden Hearing Loss: Key Factors Explained appeared first on The Microsuction Ear Wax Removal Network.